Are your calf muscles even fit enough to run?
/I’ve come to the conclusion that nearly everybody’s calf muscles stink. It’s partly a problem because runners tend to underestimate structural demand and think of the calf as a minor muscle group that doesn’t do much except push them a bit forward. Surely the big hip and thigh muscles are the real workers, right? Pushing is certainly some of the calf’s role during the later part of the running stride, in that brief moment before your foot leaves the ground. But slightly earlier in the stride, which is called mid-stance, as your body is moving forward over your fixed leg, the calf muscles are in full workhorse mode.
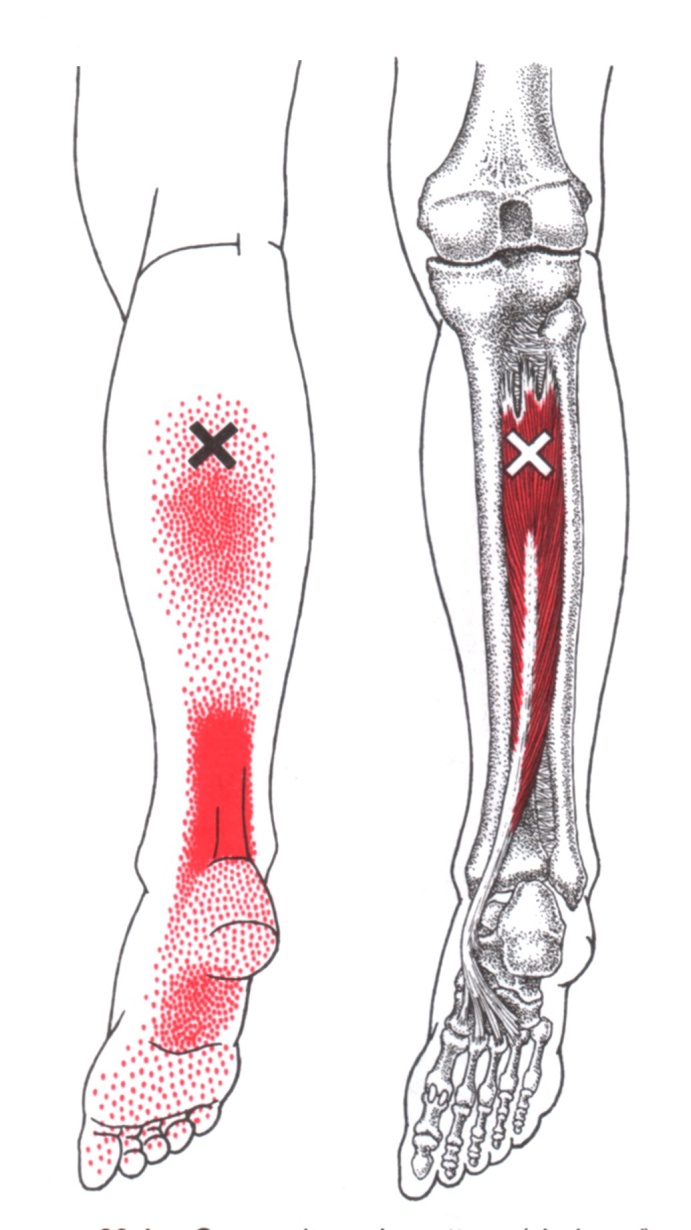
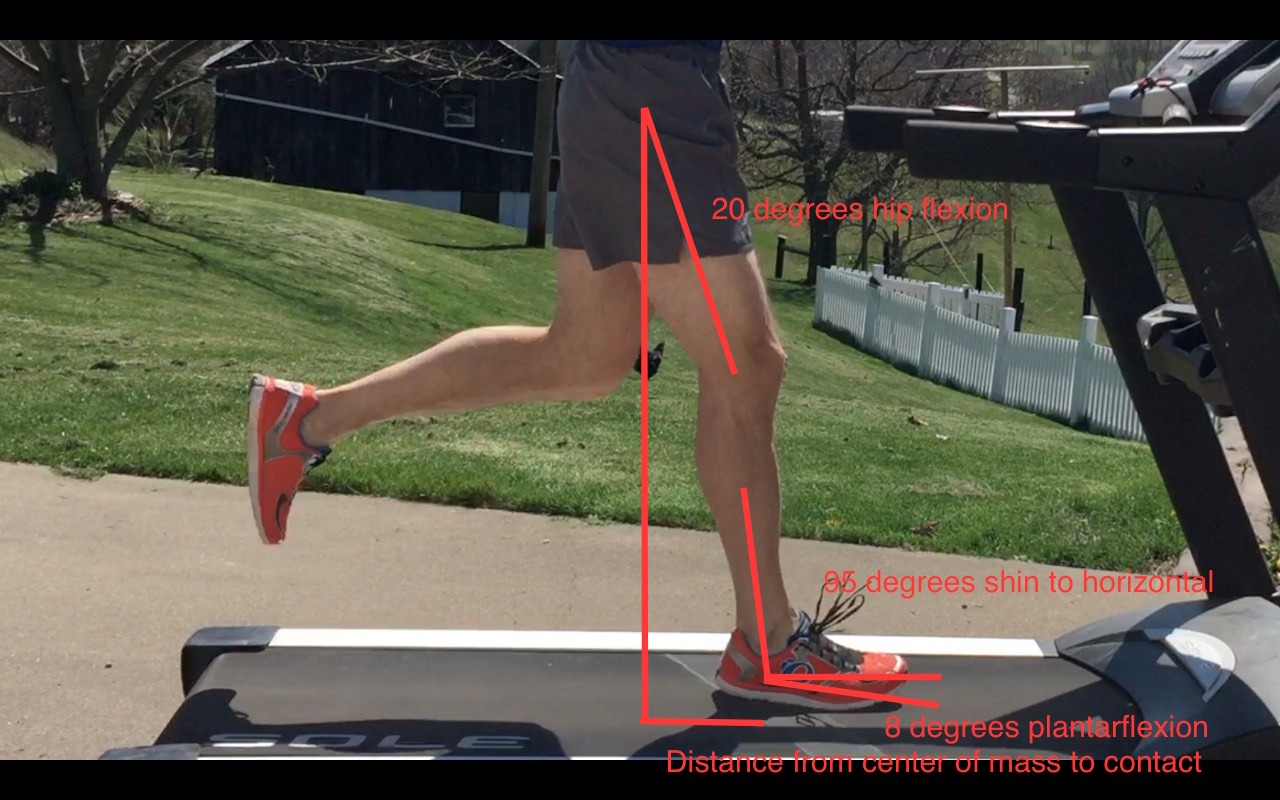
This mid-stance timing is actually the moment when the soleus, which is the biggest calf muscle, stealthily receives its peak demands. The soleus provides a major stabilizing effect to the ankle and knee, working synergistically with the thigh’s big quadriceps to keep gravity from crushing you down like Wile E. Coyote getting a boulder dropped on his head. The calf does this by resisting the forward momentum of your shin bone, using the foot as a point of fixation to work through. (Which is great if your foot does its job correctly but that’s a story for another day.)
Stop worrying about the shoe marketing hype around pronation and cushioning and start worrying about getting stronger
In 2012, Dorn et al. calculated that the soleus produced an average peak of 6 times body weight force at a 7:40 min/mile pace (7.8 mph), a pace that’s arguably quicker than many recreational folks run as they trot along. By comparison, the quadriceps were producing a measly 4 times body weight in average peak force at that pace. Doesn’t seem fair that the big thigh muscles produce less force than the smaller calf muscles does it? In that same study, speeding up to 15.7 mph (3:49 min/mile pace), a full blown sprint to most of us, resulted in an average peak of more than 8 times body weight force demands in the soleus. I know what you are thinking. That you never have or never will run that fast. Me either. Because my calf muscles suck, just like yours. (Not true, I will beat you in any calf raise test that you challenge me to as long as it’s on the moon.) The real point is that your calf muscles work ridiculously hard, even at slower paces, and speeding up further elevates their demand.
The researchers stated, “Across all running speeds, soleus, gastrocnemius and quadriceps provided roughly 75% of the total vertical support impulse needed to accelerate the body upward, with soleus contributing as much as 50%.” Notice the word vertical. The calf just wants to keep your leg tall, where your knee is bent just enough to absorb the blow of landing on the earth but not so bent that your quads work overtime or you linger on the ground too long. That’s why knee pain can relate back to less obvious factors like calf muscle function just as much, if not more so than the thigh muscles that are often blamed. And vice versa, Achilles tendon issues and calf strains can relate to poor thigh muscle function.
Older runners, especially men over 35 who make up the masters crowd, are particularly impacted by calf and Achilles tendon injuries. One unfortunate issue with age is that the Achilles tendon reduces in stiffness. I know it sounds counterintuitive at first, but research, like that from Willy in 2019, indicates that older tendons tend to have increased compliance (stretchiness) while stiff tendons do a better job at transmitting force and are less likely to be overstretched in a way that mechanically overstrains the tissue. Would you rather drive across a suspension bridge supported by slightly forgiving but very stiff steel cables or very forgiving and less stiff rubber bands? In 2017 Mahieu et al. recognized a similar situation where weaker calf muscles were even associated with Achilles tendon injury in a group of young, male military officer cadets.
Coupled with weakening calf muscles, an overzealous spring marathon training cycle can quickly turn to a puff of smoke. Once you’ve exceeded the structural capacity of the Achilles tendon and calf muscles, no amount of stretching is going to fix what you broke in that March moment of early season speedwork passion. As a side note, I really wish people would stop trying to stretch out tendon and muscle strain injuries.
Even if a person hasn’t been injured and just laid low all winter to focus on slurping [insert your beer of choice], initially adding small amounts of medium to high speed strides is the safer option for a few weeks versus going out for 2 or more miles of speedwork. In order to keep the structural and neurological capacity at a level to tolerate the highest forces, I like to have athletes perform strides year round, even if they aren’t specifically doing periodized speedwork for a target event. Strides can be short, 5 to 10 second bouts before, during, or after aerobic runs but eventually can become much longer or performed uphill to encourage even more power production while reminding your tissues that they do have a very high stress job to perform. If an endurance athlete has been hurt for a while, getting consistency and volume back are the first priority with short, slow runs. Then we can start to titrate in a little speed with strides. None of these things are appropriate, though, if the calf muscle and Achilles tendon capacity are garbage after prolonged periods of missed runs.
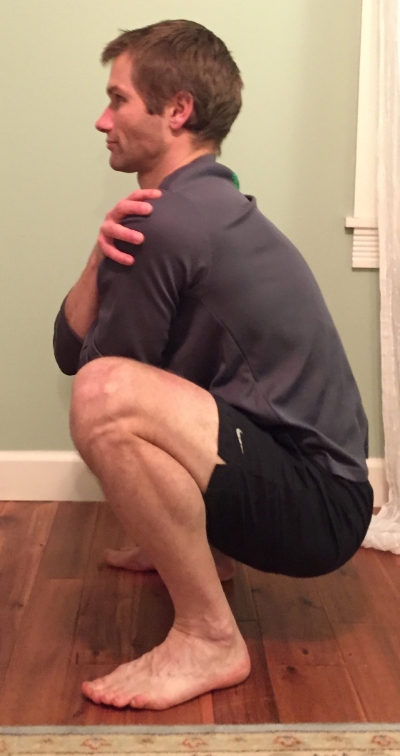
As for the nitty gritty of determining just how much your calf muscles stink? In 2017 Herbert-Losier et al. developed age-based normative values for the number of single leg calf raises that a person should be able to perform. These must be high quality (eg. full ankle motion with control) in order to count. You can see in the chart that the numbers are quite high. If I was still a spry young 30 year old, I should be able to complete 32 reps but now that I’m just about to hit that big 6-0 mark, my number is 23, which seems like a pretty high number to everyone whose last name isn’t Herbert-Losier. I’d estimate that fewer than half the people I see in the clinic are able to achieve their appropriate number. What’s your number?
Data Adapted from Herbert-Losier et al. 2017
If you aren’t making the Herbert-Losier grade but aren’t currently injured, making it a point to isolate the calf for strengthening could pay off for injury prevention. There are no guarantees, because no one is immune to injury, but there is never a penalty for being stronger. For the complete beginner, strengthening doesn’t need to be complicated. A basic double leg calf raise, knees straight, from floor height could suffice for two to three times per week for two to three weeks. The goal is to feel fatigue in the calf muscle, not pain. Once that isn’t challenging, we progress to single leg straight knee calf raises and also start to do bent knee calf raises too. The soleus works hard in both positions so don’t lose any sleep about that. Once your muscles start to come out of their coma, which could still take a few more weeks, we work toward raises on steps and raises with extra weight to further increase the resistive and range of motion demands.
Just for some perspective on how important calf strength generation is to me personally, I did single leg calf raises in straight and bent positions last week with 95# on my back for 15 repetitions in each position and of course on both legs. Sometimes I’ll do more weight, like 110-140# with reduced reps of 5-10 times. This isn’t where most runners can start and that could easily hurt many people so I’m not telling you to jump to what I do. Sometimes I go to failure, sometimes I don’t, often depending on the time of year and proximity to runs of varying stress. Other days I’ll use 20-45# as more of a light active recovery stress but that’s still too much for many beginners to start. Even still, I’ll mix in some occasional hopping and plyometric things (as long as I didn’t go really heavy) and some weighted overhead or farmer carry tip toe walking. The calf is always a point of emphasis!
May the force be with your calf muscles.
All information provided here is intended to be of a general educational nature and may not be specific to you and your needs. Unless you have seen me in the office, I am not your physical therapist. Even for the patients that I have seen, we would need to specifically assess these areas to have a full understanding of your individual capabilities. Always seek the guidance and advice of an appropriately licensed medical professional to address whether it is safe for you to perform any exercise like those mentioned here.
Resources:
https://journals.biologists.com/jeb/article/215/11/1944/10883/Muscular-strategy-shift-in-human-running
https://www.sciencedirect.com/science/article/abs/pii/S1466853X23000020
https://www.researchgate.net/publication/330309803_The_Physiology_and_Biomechanics_of_the_Master_Runner
https://www.researchgate.net/publication/315515008_Updated_reliability_and_normative_values_for_the_standing_heel-rise_test_in_healthy_adults
https://www.jospt.org/doi/10.2519/jospt.2015.5885
https://journals.sagepub.com/doi/10.1177/0363546505279918?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%20%200pubmed